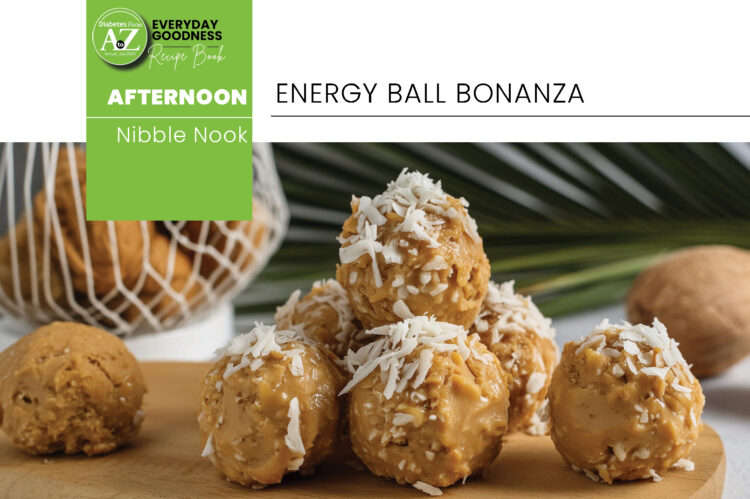
Sugar crash? Never heard of her. These energy ball bad boys are fuelled by sugar- and salt-free peanut butter and protein powder, so you can conquer your afternoon without the jitters.
Servings:
10
Ingredients:
5
Prep time:
10 – 15 minutes (excluding storing time in fridge or freezer to set)
Ingredients
- 1 ½ cup (120g) rolled oats
- 6 Tbsp. (120g) sugar- and salt-free peanut butter
- 2 scoops (about 50 – 60g) chocolate or vanilla protein powder
- 2 Tbsp. low-fat cottage cheese
- 2 Tbsp. (16g) shredded coconut, optional
Method
- Mix all ingredients in a large bowl and stir to combine. This will take some work, but it will come together as you keep mixing. Use your hands to knead if necessary.
- Once combined, take a spoonful of mixture and form into a ball. Repeat until you have formed 10 balls.
- Store in a closed container in refrigerator or freezer.

HEALTH FACT
Protein takes a while to digest so it makes you feel fuller for longer. It also helps maintain muscle mass in older people. The recommended intake is between 0.8g/kg and 1.8g/kg of body weight. Please talk to your healthcare professional before increasing your protein intake, especially if you have kidney problems as it can lead to increased strain and loss of renal function.
NUTRITIONAL INFO (per serving)
Energy 606,2kJ | Protein 10,1g | Carbs 8,8g | Fat 7,04g