Amina Goondiwala, a principal study coordinator, explains the importance and benefits of clinical trials.
The World Health Organisation has defined clinical trials as: “A type of research that studies new tests and treatments and evaluates their effects on human health outcomes. People volunteer to take part in clinical trials to test medical interventions, including drugs, cells and other biological products, surgical procedures, radiological procedures, devices, behavioral treatments and preventive care.”
Authorities of clinical trials
A clinical trial is carefully designed, reviewed and submitted to South African Health Products Regulatory Authority (SAHPRA) and ethics committees prior to being implemented at different sites. Updates during a study and at the end are also submitted to these regulatory bodies to ensure proper conducts of these studies are completed.
The Food and Drug Authority (FDA) has overall authority on trials for drugs and biologics and medical device products regulated by the agency. The purpose of an Institutional Review Board (IRB) review is to ensure that appropriate steps are taken to protect the rights and welfare of participants in the research. If the risks to participants are found to be too great, the IRB will not approve the research, or it will specify changes that must be made before the research can be done. As part of their review, IRBs consider participant inclusion and exclusion requirements to be sure that appropriate people have been identified as eligible for the trial. They often look at how and where recruitment for clinical trials will occur.
Patients’ medical records are reviewed for consideration on who can participate in a clinical trial. All patients are given an Informed Consent where the benefits and possible side effects of the medication is described. It is on a voluntary basis and a patient may stop at any time and continue with their previous treatment regime with their primary healthcare provider.
The goal of a trial is to answer specific questions on new therapies and medications. These studies are conducted in three phases and may take about 10 to 15 years before a product is approved for use in a country.
Diabetes clinical trials
Many studies have been completed for diabetes and many new trials are available for participation, not because of a last resort but to help pharmaceutical industries develop better-suited medication to control diabetes and avoid complications.
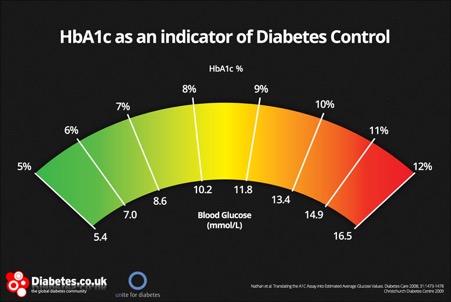
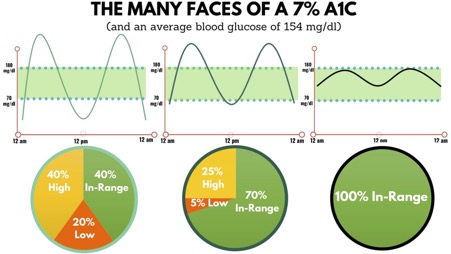
Patients with elevated glucose levels may be considered for these trials and not only will they receive medication but also have frequent clinic visits with regular blood tests and ECG monitoring. Patients may also be included in Oral Diabetic Studies or Insulin Controlled Studies.
These patients will also be contacted regularly during their scheduled visits to ask how they are feeling, and should any new symptoms develop that need to be monitored. Nurses or site staff spends time with each patient addressing their concerns regarding their conditions. Social and economic factors may also be addressed with patients having a difficult time maintaining their glucose levels. All patients are encouraged to engage in some form of exercise or activities to ensure a healthier outcome.
Benefits of participating in a clinical trial
There are many benefits to enrolling on a clinical trial. For example, you can take a more active role in your healthcare, such as learning the importance of taking your medication on time and how to deal with a hypoglycemic episode; gain access to optimal medical treatment and adherence to standard of care; get expert advice at these facilities and help others by contributing to medical research.
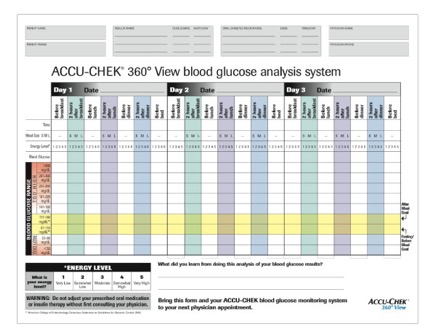
You may also involve your primary care provider on your achievements during a trial. At some facilities, they also invite family members to each appointment, so they may also learn on how to help you manage your diabetes. Eating plans where portion sizes and choosing the healthier option, specifically for diabetes, are discussed. Patients may receive glucose monitoring devices and shown how to take their glucose levels daily.
Patients are reminded that medication is not to be shared between friends and family as other diabetic patients may have other conditions as well and the prescribed medication may only be suitable to you.
Inform your treating doctor
Please speak to your primary healthcare provider prior to enrolling in any clinical trial or changing your diabetic medications. It is best to seek medical advice first before making any decisions.

MEET THE EXPERT
Amina Goondiwala is the senior study coordinator at Soweto Clinical Trials. She has 19 years’ experience in clinical trials, having participated in over 110 trials since 2002, and was awarded Study Coordinator of the Year in 2010 by the South African Clinical Research Association.
Header image by FreePik