We learn how the RetinaRisk app eliminates diabetic blindness through empowerment and predictive analytics.
The RetinaRisk app is a unique and novel tool that empowers persons with diabetes to monitor their individualised risk of developing sight-threatening diabetic retinopathy, which is one of the most common causes of blindness worldwide.
It is designed by an Iceland-based company, founded by academics and healthcare providers with over 30 years’ experience in screening, for persons with diabetic retinopathy and treating diabetes.
Diabetes stats
The global diabetes epidemic has tripled since 2000, to some 430 million persons worldwide, and is expected to exceed 600 million by 2045.
Two-thirds of persons with diabetes develop diabetic retinopathy and one-third develop sight-threatening diabetic retinopathy over twenty years. These patients are at high risk of vision impairment or even blindness if not diagnosed and treated in a timely manner.
How the RetinaRisk app works
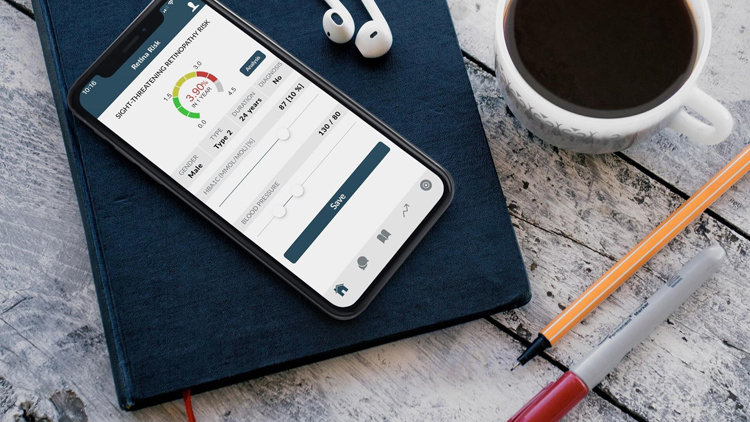
Systematic eye screening and preventive treatment are known to dramatically reduce diabetic blindness. The RetinaRisk app is a clinically-validated risk calculator that allows people with diabetes to assess, in real-time, their individualised risk for sight-threatening diabetic retinopathy, based on their risk profile, and to track the progression of the disease over time.
The app includes detailed guidelines and useful information on diabetes, diabetic retinopathy and improved self-care, which allows patients to better understand their condition and become an active participant in their own wellness journey.
The RetinaRisk app empowers persons with diabetes to become more involved in their healthcare decision-making. It supports patient self-management by demonstrating the importance of regular eye examinations and seeking timely medical assistance.
It motivates persons with diabetes to become more responsible and better-informed patients. The app’s easy-to-visualise, effective and efficient patient education tools vividly demonstrate how improvement of modifiable risk factors (e.g., blood glucose, HbA1c, blood pressure) could significantly lower the risk of potentially blinding diabetic eye disease and expensive interventions.
The algorithm at the core of the RetinaRisk app is based on extensive international research on risk factors known to affect the progression of diabetic retinopathy, such as duration of diabetes, gender, blood pressure and blood glucose (HbA1c) levels.
Clinical validation in 20 000 persons with diabetes is robust and the results have been published in several respected medical journals.
The RetinaRisk app is free of charge and our goal is to get it in the hands of as many persons with diabetes as possible around the world.